전한울
2024년 11월 15일
- 뇌내출혈(ICH)은 높은 사망률과 상당한 잔여 장애를 유발하는 심각한 상태로 현재 효과적인 급성기 치료법은 제한적이지만, 항응고 요법, 혈압 조절 및 최소 침습적 신경외과적 절차를 포함한 치료 전략에 대한 연구결과가 발표되고 있음. 2024년 현재까지 최신화된 연구 결과에 대해 정리하고 있는 논문임.
Intracerebral haemorrhage (ICH) is a devastating condition associated with high mortality and substantial residual disability among survivors. Efective treatments for the acute stages of ICH are limited. However, promising fndings from randomized trials of therapeutic strategies, including acute care bundles that target anticoagulation therapies, blood pressure control and other physiological parameters, and trials of minimally invasive neurosurgical procedures have led to renewed optimism that patient outcomes can be improved. Currently ongoing areas of research for acute treatment include anti-infammatory and haemostatic treatments. The implementation of efective secondary prevention strategies requires an understanding of the aetiology of ICH, which involves vascular and brain parenchymal imaging; the use of neuroimaging markers of cerebral small vessel disease improves classifcation with prognostic relevance. Other data underline the importance of preventing not only recurrent ICH but also ischaemic stroke and cardiovascular events in survivors of ICH. Ongoing and planned randomized controlled trials will assess the efcacy of prevention strategies, including antiplatelet agents, oral anticoagulants or left atrial appendage occlusion (in patients with concomitant atrial fbrillation), and optimal management of long-term blood pressure and statin use. Together, these advances herald a new era of improved understanding and efective interventions to reduce the burden of ICH.
Diagnosing causes of intracerebral haemorrhage
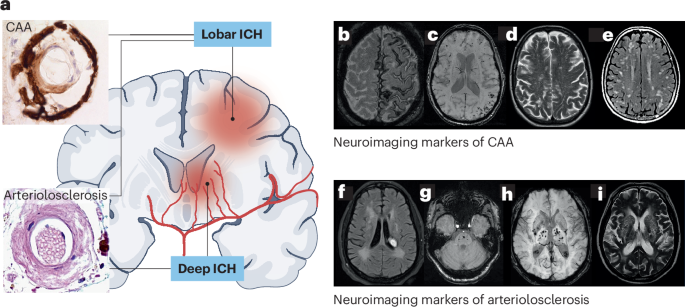
Main causes: cerebral small vessel disease (SVD), including cerebral amyloid angiopathy (CAA) and arteriolosclerosis
Macrovascular causes (~10-20%): arteriovenous malformation, aneurysm, cavernous malformation, etc.
Diagnostic work-up: brain parenchyma and intracranial vasculature imaging
CT angiography as first step, intra-arterial digital subtraction angiography as reference standard
Neuroimaging markers of SVD
CAA markers: cortical superficial siderosis, lobar cerebral microbleeds, enlarged perivascular spaces
Arteriolosclerosis markers: deep ICH, periventricular white matter hyperintensities, deep cerebral microbleeds
'Mixed' pattern: presence of both CAA and arteriolosclerosis markers
Genetics and intracerebral haemorrhage
APOE polymorphisms: ε2 and ε4 associated with increased ICH risk
Other genetic variants associated with lobar and deep ICH
Monogenetic conditions in young-onset CAA and SVD
Less common SVD subtypes
CAA-related inflammation (CAA-ri)
Iatrogenic CAA due to prion-like transmission of amyloid-β
Fluid biomarkers in diagnosis and prognosis of SVD
Neurofilament light chain (NfL) and glial fibrillary acidic protein (GFAP) as potential blood biomarkers
Cerebrospinal fluid (CSF) examination for CAA diagnosis
Current classifications for intracerebral haemorrhage aetiology
SMASH-U and H-ATOMIC classifications
CLAS-ICH and CADMUS classifications based on neuroimaging features
Advances and uncertainties in acute therapy
Therapeutic targets
Primary injury: direct damage from ICH
Secondary injury: haematoma expansion, inflammation, oedema
Key treatment goals: preventing haematoma expansion and reducing secondary injury
Medical treatment for intracerebral haemorrhage
Blood pressure management: target <140 mmHg within 1 h of ICH onset
Antithrombotic reversal: stopping antiplatelet/anticoagulant medications
Haemostatic agents: tranexamic acid, recombinant activated factor VIIa
Anti-inflammatory treatments: under investigation
Surgical treatment of ICH
Minimally invasive surgery showing promise in improving functional outcomes
Ongoing trials investigating optimal surgical techniques and timing
Decompressive craniectomy: potential benefit in selected cases
Advances in prevention measures
Recurrent intracerebral haemorrhage
Higher recurrence risk in lobar ICH and CAA
MRI markers of SVD help assess recurrence risk
Recurrent ischaemic stroke
Annual risk similar to recurrent ICH (1-4%)
Higher risk in arteriolosclerosis-related ICH
Long-term blood pressure control
Key for secondary prevention in both deep and lobar ICH
Ongoing trials investigating optimal blood pressure targets
Antiplatelet and anticoagulation therapy after intracerebral haemorrhage
Antiplatelet therapy: RESTART trial showed no increased risk of ICH recurrence
Anticoagulation: ongoing trials assessing safety and efficacy in atrial fibrillation patients
Utility of left atrial appendage occlusion
Potential alternative to anticoagulation in ICH patients with atrial fibrillation
Ongoing trials comparing LAAO with medical therapy
Statins and other lipid-lowering drugs
Controversial use in ICH patients
Ongoing SATURN trial investigating statin continuation vs. discontinuation after ICH
Disease-modifying therapies in cerebral small vessel diseases
Intensive blood pressure management for arteriolosclerosis
Potential therapies for CAA: anti-amyloid antibodies, RNA interference
Anti-inflammatory approaches under investigation
Conclusions and future directions
Advances in understanding ICH mechanisms and potential treatments provide optimism
Improved classification of underlying aetiologies
Ongoing trials in acute management and secondary prevention
Need for implementation of integrated care pathways and organization of care
Future studies based on improved understanding of ICH disease mechanisms and natural history